How stem cell transplants help cure bone marrow failure syndromes
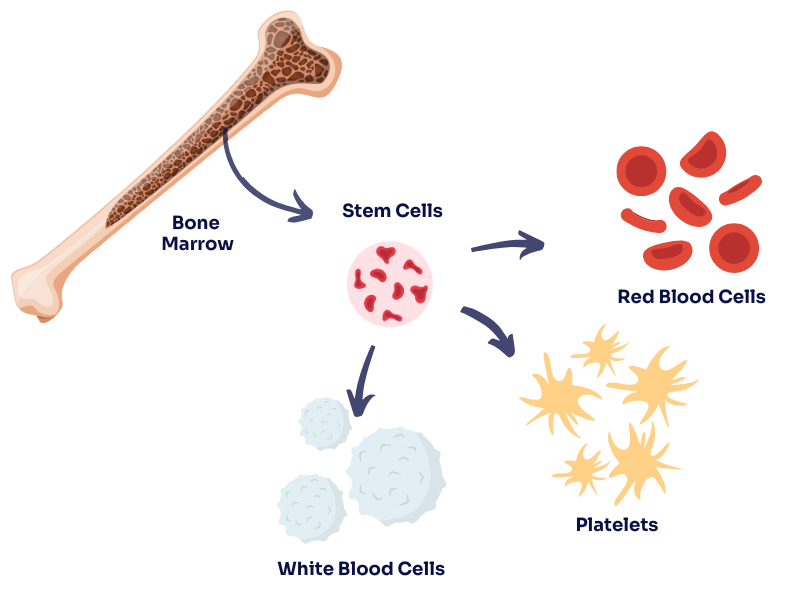
Our bone marrow is like a factory inside our bones. It produces the blood cells our bodies need to survive—red blood cells that carry oxygen, white blood cells that fight infections, and platelets that help blood clot. But sometimes, this factory stops working properly. This is called a bone marrow failure syndrome, and it can be life-threatening.
What causes bone marrow failure?
Bone marrow failure can happen for different reasons. Some people are born with conditions that affect their bone marrow (these are called inherited syndromes), while others develop problems later in life (these are called acquired syndromes).
Some common causes include:
- Aplastic anaemia – The bone marrow stops making enough blood cells. This can happen because of an immune system attack, exposure to certain chemicals or medications, or for no clear reason.
- Fanconi anaemia – A rare genetic condition that causes bone marrow failure, often in childhood.
- Dyskeratosis congenita – Another inherited condition that affects bone marrow and other parts of the body.
- Myelodysplastic syndromes (MDS) – A group of disorders where the bone marrow makes faulty blood cells that don’t work properly.
When the bone marrow isn’t working, people can become very sick. They may feel weak and tired because of a lack of red blood cells (anaemia), bruise or bleed easily because of low platelets, and get infections more often because they don’t have enough white blood cells.
How does a stem cell transplant help?
A stem cell transplant (also known as a bone marrow transplant) is a way to replace the damaged bone marrow with healthy stem cells from a donor. Stem cells are special cells that can grow into different types of blood cells. When a person receives a stem cell transplant, the donor’s healthy cells travel to the bone marrow and start making new, working blood cells. It’s like replacing a broken factory with a brand-new one.
For many people with bone marrow failure syndromes, a stem cell transplant is the only cure. Without a transplant, their body may never produce enough healthy blood cells on its own. While the process can be challenging, it offers the chance for a new start—a future without the constant risks of severe anaemia, infections, or bleeding.
The process of a transplant:
- Finding a donor – The best match usually comes from a family member, but if no match is found in the family, doctors look for an unrelated donor on the stem cell registry – that’s us.
- Preparing for transplant – The patient receives chemotherapy (and sometimes radiation) to remove the faulty bone marrow and make space for the new stem cells.
- Receiving the new stem cells – This is done through a transfusion, similar to receiving blood. The donor’s stem cells travel to the bone marrow and begin to grow.
- Recovery – It takes time for the new stem cells to start producing enough blood cells. Patients need close monitoring to prevent infections and other complications.
Every committed donor brings a patient one step closer to a cure
Not everyone who needs a transplant can find a perfect donor match. That’s why having a diverse and committed pool of donors on the stem cell registry is so important. The more people who join, the greater the chance that someone with a life-threatening bone marrow failure syndrome will find the match they desperately need.
But signing up isn’t enough—commitment matters. Unlike blood donation, where you donate immediately, being on the stem cell registry means you could be called to donate in the future—sometimes years after joining. If that happens, it means you’re the best or only match for a patient whose life depends on you saying yes. But if too many donors decline, can’t be reached, or aren’t truly prepared to follow through, patients are left with fewer options—or no hope at all.
Every person who joins the registry represents real hope for someone in need. But that hope only becomes reality when donors stay informed, contactable, and ready to take action when it counts. If you’re 18–35, in good health, and willing to make a real difference, consider joining today—you could be the cure for someone with a bone marrow failure syndrome.
